The image above captures financial information about Canterbury Rehabilitation (known as Lexington Court until new ownership this year) published on the Virginia Health Information website for the fiscal year ending Oct. 31, 2018. That is the most recent data available to the public.
Canterbury, to refresh your memory is the privately owned Henrico County nursing home for Medicaid patients where the COVID-19 virus has killed 46 patients so far — the deadliest outbreak in any facility in the country. It is a national scandal that cries out for explanation. One angle worth exploring is whether the nursing home could have afforded to hire additional nurses, and whether better staffing could have prevented or slowed the spread of the disease.
I can’t answer the latter question, but the VHI data allows us to address the former. If we compute the nursing home’s operating margin by dividing operating income of $876,728 by operating revenue of $15,132,121, we get an operating margin of 5.8%. That is a healthy margin for a Medicaid nursing home.
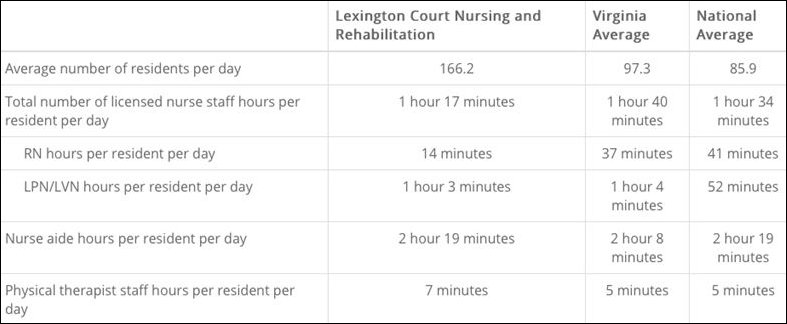
Now, if we review staffing levels, updated on March 31, 2020, as found on VHI, we see that Canterbury/Lexington Court needed two additional RNs to reach the national average RN hours per resident per day of 41 minutes.
Had Canterbury hired another Level One RN (right out of nursing school), it would have incurred additional cost of roughly $103,000 — $63,400, the median nursing salary in Virginia, plus $40,000 more to cover administrative and benefit costs. That done, Canterbury (Lexington Court) would have made $773,728 that year, producing an operating margin of 5.1%, still very healthy. Had the nursing home hired two Level One RN’s, the operating margin still would have been a respectable 4.4%. Perhaps management tried to hire and no candidate applied. We don’t know. It’s worth finding out.
So, why did Canterbury/Lexington Court not hire more nurses? Did the state order the nursing home to do it and it the nursing home fail to comply? The state has the relevant inspection reports and, if it is doing its job, letters of correction. The Commonwealth should release that information to the press. If not, a FOIA request can sort it out.
[1] salaryhttps://www.salary.com/research/salary/alternate/registered-nurse-rn-level-1-salary/va

Leave a Reply
You must be logged in to post a comment.