 by James C. Sherlock
by James C. Sherlock
I have written often of the costs of (1) avoidable emergency care and (2) avoidable hospital admissions for chronic diseases.
Each type of excess costs could be prevented by timely visits to primary care practitioners and following their prescriptions for treatment.
The avoidable costs are largely paid by Virginia’s Medicaid program run by Virginia’s Department of Medical Assistance Services (DMAS). DMAS pays Managed Care contractors to diminish these costs and improve the health of the communities in which its clients live. That program has not worked as well as it should.
There is a proven better way: Maryland’s Health Enterprise Zones (HEZ) program.
Virginia needs better financial data to support budget impact assessments for legislation to go down that path. The VDH data contractor has proven with its calculation of avoidable emergency department visits that both the data and the methodology are available to accomplish that same approach to avoidable hospital admissions.
We did not have those calculated figures when then-Delegate Jason Miyares and I tried and failed to establish a HEZ pilot program in Virginia a few years ago. Then, we had just rough estimates. The bill was passed overwhelmingly in the subject matter committees but buried in the House Appropriations Committee.
VDH should direct its contractor to make the calculations soon that are required to support 2023 legislation.
Avoidable Emergency Department visits. Virginia Health Information, the VDH data contractor, has reported data on potentially avoidable emergency department (ED) visits in 2020.
An emergency department visit is considered potentially avoidable when the care provided may have been more appropriately managed by a primary care practitioner (PCP) in a lower cost setting, such as a physician’s office.
Of the 113,464 potentially avoidable ED visits, 88% were for:
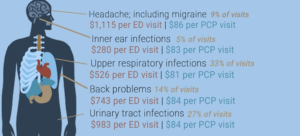
The total costs for the potentially avoidable visits in 2020 was $75 million. Total cost for similar care by a PCP in 2020 was $8.3 million. Potential savings in one year: $66.7 million.
These visits have a large impact on the cost of healthcare for all Virginians. Using data from the Virginia All Payer Claims Database (APCD), Virginia Health Information identified that about 10% of the 1.1 million ED visits in 2020 may have potentially been avoided and treated with lower cost healthcare in a PCP’s office.
Avoidable ED visits represent the far smaller of the two areas of wasted money that could be avoided by better availability and use of PCPs. Even if one did not care about the health of the patients, which we do.
Avoidable hospital admissions costs from untreated chronic diseases dwarf unnecessary ED visit costs to Medicaid in other states.
Maryland HEZ program. Massive reductions in unnecessary hospital admissions were achieved by Maryland’s Health Enterprise Zone (HEZ) program. The net savings to Medicaid there were enormous.
In a four-year pilot with just five small HEZ zones in Maryland, the following findings were reported by Johns Hopkins University. All data refer to the small four-year pilot program only.
In this quasi-experimental study, we found that HEZ Initiative is associated with a reduction of 20,955 inpatient stays during 2013 to 2016.
Unexpectedly, ED visits increased by 39,427.
But:
- We estimated the net savings to the health care system was $109.15 million.
- Impact on Maryland Economy: + $27.6 million
- Total State investment : $16.4 million.
- State financial gain : $135.75 million.
The state financial benefit-to-cost ratio measured over 4 years was 8.28/1.
How about the opinions of the residents of these HEZs?
Findings from Resident Interviews
• Majority of residents were either very satisfied or satisfied with the services they received.
• Residents believed the HEZ objectives were meeting community needs.
• Residents felt the biggest impact of the HEZ initiative was to improve access to health services and chronic condition management.
• Residents felt the HEZ helped them improve their health behaviors
The purpose of establishing the Maryland HEZs was to target state resources to:
- Reduce health disparities among racial and ethnic groups and geographic areas;
- Improve health care access and health outcomes in underserved communities; and
- Reduce healthcare costs and hospital admissions/readmissions.
Those costs are not avoided and the other two goals not nearly as well achieved by Virginia’s Medicaid Managed Care program.
What next? Perhaps we should try the Maryland approach, but we will need data to provide the budget impact.
To provide the as-is cost baseline, I suggest VHI for VDH and DMAS quantify the costs of avoidable 2020 hospital admissions in Virginia as it now has quantified the costs of avoidable ED visits.
Compute both total costs and Medicaid costs for both categories.
Together, those figures, even without computing, as did Maryland, the positive impact on the state economy, will provide a financial benchmark to support budget impact assessments for HEZ legislation.
The Health Insurance Reform Commission should take the lead in asking for a brief on those Virginia data, the Maryland Health Enterprise Zone (HEZ) results certified by Johns Hopkins and the very large positive implications for Virginia.
Bills with positive net budget impact are appropriate even in a non-budget year.
More than appropriate in this case.

Leave a Reply
You must be logged in to post a comment.