
by Carol J. Bova
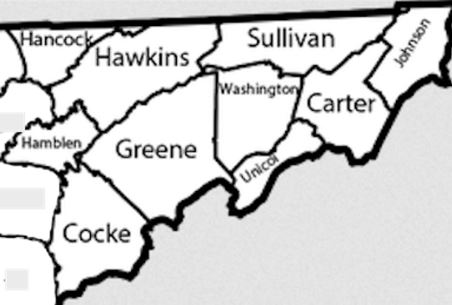
When Mountain States Health Alliance and Wellmont Health System merged to create Ballad Health in 2018, the healthcare companies justified the consolidation with the argument that the ability to cut costs and rationalize delivery of health services would yield tangible benefits to patients in Southwest Virginia and Northeastern Tennessee.
The previous article in this series, “Cuts and Consolidations,” detailed how Ballad Health bolstered finances through shared value-based payment savings, bond refinancing, staff reductions and closures of off-site facilities. This article, Part III, shows how the company acted to lower costs and enhance revenue by consolidating medical services, repurposing hospitals, introducing telemedicine, and implementing a new IT system.
The Virginia Cooperative Agreement, which outlined the requirements of Virginia regulators, allowed repurposing as long as certain “essential services” were retained. Deploying telemedicine and rotating specialty clinics in rural hospitals would help it meet the requirement.
An example of successful repurposing was the reallocation of service lines in Wise County after three facilities came under the same corporate umbrella. Ballad moved Mountain View Regional Hospital’s emergency department to nearby Norton Community Hospital and its inpatient services to Lonesome Pine Hospital just a few miles away. The company then transferred Norton’s inpatient rehabilitation center to Mountain View to strengthen it as a skilled nursing and long-term-care facility. The Centers for Medicare and Medicaid (CMS) gave Mountain View an above-average 4-star rating in its Nursing Home Compare site.
A necessary component of Ballad’s plan was the installation of a $200 million system-wide technology platform, Epic, which required the training of 6,000 Ballad employees and health partners. Epic provides electronic health records for all inpatient and outpatient services for in-person or tele-visits and allows direct scheduling of patient appointments. Although the Cooperative Agreement called for conversion to be completed by June 2020, it was delayed eight months by the pandemic and not completed until November, 2020.
The plan was for Telehealth services to cover primary care visits and specialty care in pain management, neurology, cardiology, pediatric endocrinology and behavioral health. Other specialty support would be available to doctors at hospitals throughout the region. School nurses in the region would have telehealth support from pediatric specialties, too.
The success of telehealth visits and consultations hinges in part on efforts to expand internet access and affordability across the region. Virginia Business reported in January 2021 that the Virginia Telecommunication Initiative (VATI) approved a $16.2 million grant to provide access to 8,335 units, including 82 businesses, in Buchanan, Dickenson, Russell and Tazewell counties, plus another $1.23 million for fiber in Lee County for 679 total units. A previous $455,000 grant to Russell County was part of the cost to provide service to about 600 units. Despite the subsidies, the estimated cost to subscribers ranges between $90 to $180 per month — beyond the means of many Ballad patients in need of primary medical care.
According to Virginia regulators, Southwest Virginia had significant gaps in inpatient hospital services. Among other initiatives, Ballad Health agreed to provide essential services in Lee County, where the community hospital had shut down in 2013, “until such time as a hospital is open and fully operational” and opened an urgent care center in 2019.
Ballad will offer in-house telehealth as part of reopening Lee County Hospital. The 10-bed critical access hospital is expected to open in July after a major reconstruction to bring it up to current medical facility standards. On February 24, 2021, Ballad Northwest Market President Lindy White was quoted by News Channel 11, WJHL as saying, “The upgraded facility in Lee County will offer telehealth options in-house and help connect patients with specialists in other regions.”
Another big challenge for Ballad was tackling the region’s opioid epidemic. The Virginia Merger Monitor’s First Report in January 2020 said that “30 percent of the babies born in Wise County are born addicted. Ballad is starting to address these needs.”
Ballad also consolidated services at two Greeneville, Tennessee, hospitals. Urgent care, inpatient services and surgical services were concentrated in one facility, while the other was repurposed “as a residential facility for women who are pregnant or parenting and struggling with the issue of addiction.” This Strong Futures program began accepting applications on February 1, 2021.
Tennessee gave Ballad a $7 million grant toward the first two years’ expenses. Unfortunately for Virginia, the program is available only to women in Tennessee.
When Dennis Barry, the Virginia Merger Monitor, and Jeffrey Mitchell, attorney for the Southwest Virginia Health Authority, were asked, “Is there anything in the works for Virginia pregnant women or mothers needing addiction recovery services,” they were forwarded Ballad Health’s Report to Our Communities.
The report doesn’t answer the question. Perhaps the plan is for telemedicine behavioral health visits. Ballad spokesperson Stacey M. Ely has not replied to emails that Bacon’s Rebellion sent in March, so we don’t know.
The 16 Quality Measures for hospitals are aimed at reducing accidental harm to patients, such as pressure ulcers, falls resulting in a broken hip, hospital-acquired infections, and other post-surgical issues. Most Ballad reports of system-wide averages show improvement over the 2017 baseline. How are the individual Virginia hospitals doing?
We will address that question in Ballad Merger IV: Has Hospital Quality Improved?
Carol Bova is a writer living in Mathews County.

Leave a Reply
You must be logged in to post a comment.