by Carol J. Bova
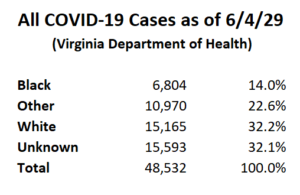
Discussion of the percentage of black COVID-19 hospitalized patients in Virginia is based on the known racial identification of all COVID-19 cases. The breakdown of all cases shows this is a false narrative. We don’t know what the true racial percentages are because currently 32% of all COVID-19 cases have no racial identification.
 From here forward, that problem should be reduced by new federal guidance announced on June 4 requiring labs to report demographic data like race, ethnicity, age, and sex.
From here forward, that problem should be reduced by new federal guidance announced on June 4 requiring labs to report demographic data like race, ethnicity, age, and sex.
Today, the U.S. Department of Health and Human Services (HHS) announced new guidance that specifies what additional data must be reported to HHS by laboratories along with Coronavirus Disease 2019 (COVID-19) test results. The Guidance standardizes reporting to ensure that public health officials have access to comprehensive and nearly real-time data to inform decision making in their response to COVID-19. As the country begins to reopen, access to clear and accurate data is essential to communities and leadership for making decisions critical to a phased reopening.
“The requirement to include demographic data like race, ethnicity, age, and sex will enable us to ensure that all groups have equitable access to testing, and allow us to accurately determine the burden of infection on vulnerable groups,” said ADM Brett P. Giroir, MD, Assistant Secretary for Health. “With these data we will be able to improve decision-making and better prevent or mitigate further illnesses among Americans.”
It’s good that solid information will be available. It’s a shame that the Commonwealth failed to require the same information sooner. We can hope public health officials will support the effort now.
Carol J. Bova is a writer who lives in Mathews County.

Leave a Reply
You must be logged in to post a comment.