by James A. Bacon
Now that the COVID-19 virus has arrived in Virginia, key institutions are reacting. Several universities are extending their spring breaks; others are shifting to online classes. Event organizers are cancelling their events, from book fairs to health fairs. Major employers are telling employees to work remotely. Jails are suspending visitations to inmates. Hospitals and nursing homes are restricting the number of visitors.
That’s exactly what it takes to slow the spread of the coronavirus. There is no stopping the virus, as highly contagious as it is, from reaching epidemic proportions in the state, The strategy is to delay, delay, delay, thus avoiding a surge of severely ill patients to hospitals that lack the capacity to handle them. Realistically, the best case scenario is to spread out the epidemic temporally to minimize the number of COVID-19 patients treated in hospitals at any given time. (See the graph in Don Rippert’s most recent post here to get a visual sense of how this works.)
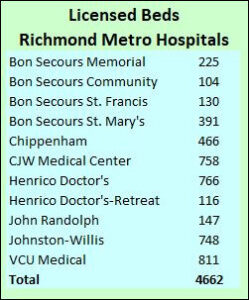
By my count, there are 4,662 acute-care hospital beds in the Richmond region within 20 miles of downtown. According to national figures, the bed occupancy rate runs slightly above 70%. That’s better than in the 1990s when national healthcare policy deemed high bed utilization rates a key to controlling health care costs and occupancy rates ran above 90%.
Correction: The table above includes double-counted beds for HCA hospitals. Chippenham and Johnston-Willis are part of CJW Medical center, while Henrico Doctor’s-Retreat is part of Henrico Doctor’s. A more accurate account of licensed acute care hospital beds in the Richmond region is 3,333. I have not amended the text below to reflect these numbers.
If we assume that 30% of the Richmond region’s hospital beds are empty on average, that implies that local hospitals have about 1,400 beds to spare. Is that enough?
That depends on how fast the coronavirus spreads, and what percentage of the population experiences acute distress. About 15% of the cases in China required hospitalization. On the optimistic premise that Americans on average have fewer risk factors than the Chinese — less air pollution, fewer smokers — let’s assume that only 10% of Americans who contract the disease are ill enough to warrant admission into hospitals. (That may be optimistic, however, because our population is older; an 80-or-older age is a significant risk factor.)
The Richmond region has a population of about one million. If half the population is infected, and if 10% of those infected are admitted to the hospital, that implies hospitals will have to contend with 50,000 coronavirus patients.
Fifty thousand patients, 1,400 beds. Let that sink in.
Hospitals can free up some beds by rescheduling discretionary medical procedures, but even if they emptied their rooms of every current patient, there still would be a vast gulf between supply and demand. I have not checked the licensed-bed numbers for hospitals outside the Richmond region, but I expect the pattern is similar.
If social-distancing strategies can delay the spread of the coronavirus over, say, 26 weeks, that implies about 2,000 additional hospitalizations per week. That would overload Richmond-area hospitals, but not too severely. But if social-distancing is too little, too late, and if the region experiences a geometric rate of increase as seen in other countries, we can envision hospitals getting swamped by 5,000 to 6,000 weekly.
Where will those patients go? What preparations are being made in anticipation of such a surge? This question is fundamental to Virginia’s response to the pandemic.
So far, we have heard nothing from the Northam administration or Virginia’s hospitals on what measures they are taking to expand capacity. And so far, Virginia’s established-media coverage of the coronavirus has been limited mainly to regurgitating press releases. Insofar as Virginia journalists have been inquisitive, they have focused on the shortage of testing kits, a second-tier problem.
For now, it seems, combating COVID-19 is up to the citizenry — employers, churches, event organizers, schools, and private citizens — to take every conceivable precaution in the hope that we can slow the plague’s inevitable onslaught and buffer the impact on our hospitals.

Leave a Reply
You must be logged in to post a comment.