When I first read of the racial differences in Virginia’s COVID-19 statistics, I wondered how reliable the numbers were. After exploring details from multiple sources, medical and popular, I no longer doubt there is a serious demographic divide in the impact of COVID-19. The disparities are is not limited by race but tie into genetics and early life experience. Socioeconomic status, especially early in life, is too often the foundation for adult impacts of health conditions that increase the risk of severe COVID-19.
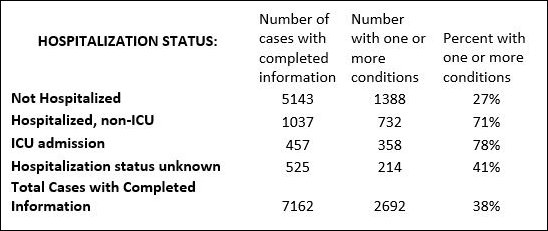
Diabetes, chronic lung disease (including moderate to severe asthma, heart disease, obesity, and other chronic diseases are the top four comorbidities for COVID-19, according to an April 3 CDC report. Others include an immunocompromised condition, kidney disease requiring dialysis, pregnancy, being a current or former smoker, neurologic disorders, and liver disease.(1) The report broke down 7,162 COVID-19 cases with “data on the presence or absence of underlying health conditions and other recognized risk factors for severe outcomes from respiratory infections.”(2) Although the results were preliminary and limited by the amount of data collected by health departments, they seem to echo more recent reports.
In that first study of 7,162 COVID-19 cases with completed information on one or more underlying conditions, the CDC found:
On April 17, CDC issued advice to groups at higher risk for severe illness on why each type of comorbidity puts them at higher risk and what actions they should take.(3)
“The Lancet” published a report on March 16, “COVID-19: consider cytokine storm syndromes and immunosuppression.”(4) The article discussed screening for patients with severe COVID-19 “to identify the subgroup of patients for whom immunosuppression could improve mortality.” This screening advice seems to have been overlooked in the rush to try immunosuppressants like chloroquine and other rheumatoid arthritis drugs. Fortunately, chloroquine is becoming available again for with RA and lupus who depend upon it for relief of their conditions.
“Physicians Weekly” posted an article on April 8, “Cytokine Storm: The Sudden Crash in Patients with COVID-19” that describes the “overproduction of immune cells and their activation compounds–cytokines….” which “can lead to respiratory distress and increases the risk of mortality in patients.” (5)
There has been a flurry of articles recently on cytokine storm. One article today (April 21) in The Atlantic, (6) covers the topic in clear English and goes on to explore the CDC report that found significantly higher death rate for Latinos and African Americans than for white Americans. “Rates of death and severe disease are several times higher among racial minorities and people of low socioeconomic status.”
For now, the screening and treatment described in “The Lancet” article must be applied to those COVID-19 patients at high risk to improve their chances of survival.
But there is no instant formula for improving early life experiences. Current medical and educational attempts cannot do all that is needed. Long-term change in lifestyle and attitudes must come from within a culture, not imposed from outside. Perhaps the best hope is for community organizations, churches, or fraternal groups to be part of the change in developing leaders who are respected and can influence those in their community to guide their children to better lifestyle choices that will reduce their long term health risks.
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/underlying-conditions.html
- https://www.cdc.gov/mmwr/volumes/69/wr/mm6913e2.htm
- https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30628-0/fulltext
- https://www.physiciansweekly.com/cytokine-storm-the-sudden-crash-in-patients-with-covid-19/
- https://www.theatlantic.com/health/archive/2020/04/coronavirus-immune-response/610228/
Carol J. Bova is a writer in Mathews County and on the staff of
Chesapeake Style magazine.

Leave a Reply
You must be logged in to post a comment.