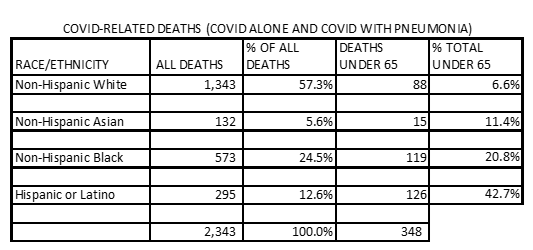
The Centers for Disease Control (CDC) death certificate reports are the one reliable indicator of the impact of Covid-19 on the various population groups in Virginia. The CDC racial/ethnic breakdown from 2/1/20 to 7/4/20 of all deaths from COVID-19 alone, together with COVID-19 and pneumonia, shows Virginia Hispanics accounted for 12.6% of all COVID-19 deaths. That does not appear to be far out of line with a 10% Hispanic population in the Commonwealth in 2018, especially when allowing for an unknown number of undocumented Hispanic persons plus Hispanic population increases since then.
What is shockingly out of line is the CDC Virginia death certificate numbers show 42.7% of Hispanic COVID-19 deaths within the 35- to 64-year-old age bracket, as shown in the chart above.
Why has this happened? Are comorbidities like diabetes, auto-immune conditions or obesity responsible?
Hispanic workers are known for their work ethic. Is that part of the reason for these numbers? Did they continue working out of economic necessity or dedication? How many worked in long term care facilities and how many in meat or poultry production?
Were those who died at these younger ages living in substandard housing?
Did they not seek health care before the virus caused a catastrophic illness, or was treatment ineffective?
Were they undocumented and afraid to reveal their illness?
Were there other reasons?
Everyone needs to stop blaming systemic racism as a cause and relying on news media and politicians posturing about inequities. We need to demand the Office of Health Equity investigate and document the facts and then formulate real life solutions.
Carol J. Bova is a writer residing in Mathews County.

Leave a Reply
You must be logged in to post a comment.