
by James C. Sherlock
Sentara Health, once described by The Washington Post as “playing COPN like a violin,” yesterday went statewide with an acknowledgment that its system is out of capacity for many who seek its help.
On a Zoom press conference yesterday, Sentara reported seeing a huge surge in hospital admissions. Hospitalizations have more than tripled since Dec. 26. That is combined with a depletion in hospital staff caused by illness.
Dr. Jordan Asher, Sentara’s chief physician executive, said:
We take care of people that are sick. You’re coming around unvaccinated versus vaccinated does not come into play as we think about it. As resources get scarce, do you triage differently? Obviously the answer to that is yes … but we have a very strong way of going through all that, of looking at that. We’re used to that.… How we think about the utilization of resources and how we think about triaging is part of our everyday work. (Bolding added by author)
So you might find yourself on the down side of emergency room triage. Not good being you.
Let’s see, perhaps some Hampton Roads patients can go to DePaul Hospital in Norfolk. No, sorry. It closed under assault on its business by a certain regional monopolist.
Perhaps Arlington patients could go to Northern Virginia Community Hospital. Sorry, it too is closed.
COPN (Certificate of Public Need) rulings required it to be bought and closed in 2006 in order for a new hospital to be built in Loudoun County. You could not make that up.
Leesburg is 30 miles — perhaps an hour optimistically — from Arlington in legendary Northern Virginia traffic.
Unless it snows.
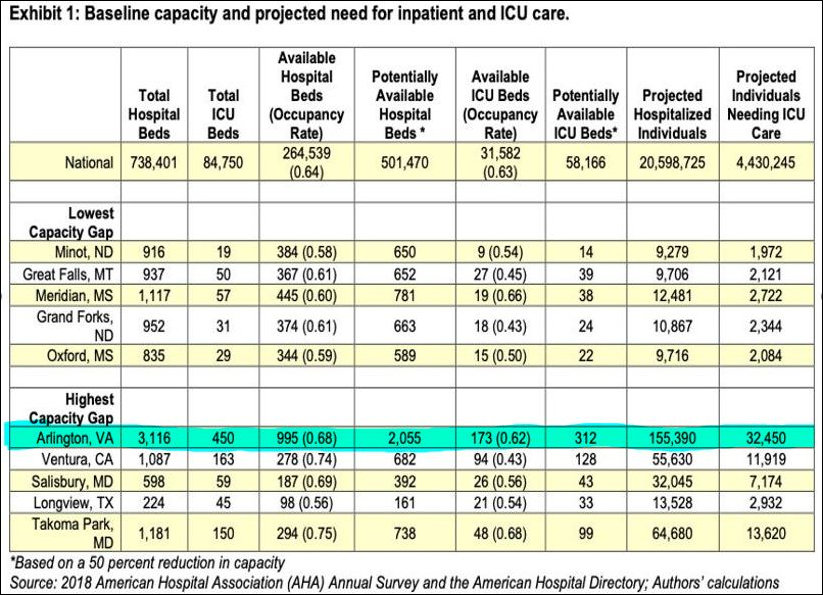
That left Arlington with the highest hospital capacity gap in America as assessed by the American Hospital Association at the onset of COVID in 2020.
Personal note: A close family friend was scheduled for a hip replacement next week in a Sentara hospital here in Hampton Roads. Cancelled. Lack of capacity.
The magic of COPN. So there are no options. By design.
Who knew? Q. Who could have guessed that COPN would limit capacity below what is needed for emergencies? A: nearly everyone with knowledge of the industry other than Virginia’s hospital monopolies. More correctly: they knew it also, but the answer did not fit their business model.
When the General Assembly convened one of a seemingly endless series of Certificate of Public Need workgroups in 2015, the final report it published in December of 2015 cited an input from Dr. Donald Adam:
He stated that additional access to emergency medical care is needed across the nation and in Virginia. He argued that COPN does not allow this additional access as it restricts expansion.
Then there was the Joint Statement of the Federal Trade Commission and the Antitrust Division of the U.S. Department of Justice submitted to that same working group on October 26, 2015.
CON laws, when enacted, had the laudable goals of reducing health care costs and improving access to care. However, it is now apparent that CON laws can prevent the efficient functioning of health care markets in several ways that may undermine those goals. First, CON laws create barriers to entry and expansion, limit consumer choice, and stifle innovation. Second, incumbent firms seeking to thwart or delay entry by new competitors may use CON laws to achieve that end. Third, as illustrated by the FTC’s recent experience in the Phoebe Putney case, CON laws can deny consumers the benefit of an effective remedy following the consummation of an anticompetitive merger. Finally, the evidence to date does not suggest that CON laws have generally succeeded in controlling costs or improving quality. (Bolding addled by author).
That joint statement input was from the Obama administration.
The final report noted:
The Virginia Hospital and Healthcare Association (VHHA) established a COPN Task Force in order to conduct its own review of the COPN process and develop specific recommendations corresponding to each item in the study mandate. VHHA issued an initial report of findings and recommendations in June 2015. This report references the VHHA report in various sections.
So, the hospital monopolies developed a different view than everyone else. That view of course carried the day. Both the General Assembly and the Department of Health have been under the sway of the VHHA for 40 years.
The warnings were disregarded. Nothing changed. And here we are.
Virginians have reaped what our political class has sown.

Leave a Reply
You must be logged in to post a comment.